
Allergies are fairly common and growing, especially in children.
The prevalence of food allergy is a lot higher in kids under 5 years of age, than those ages 5 to 17 years.
A 2008 study by CDC found 4 out of every 100 children had some kind of food allergy.
This study also found that food allergies among children are increasing. For example, they increased by 18 percent within ten years of their study, starting in 1997.
Unfortunately, food-allergy-related hospitalizations among children also increased from 1998-2000 through 2004-2006.
These numbers have real impact on quality of life: children with food allergies are also more likely to have asthma or other allergic conditions. This increases the work needed for raising kids among new moms and their families.

Figure: Hospitalizations due to food allergies are rising, according to a CDC study.
Food can make one sick in many different ways. It may cause an immune response or the body might find it hard to digest, or it might be contaminated with toxins from bugs and pathogens.

Figure: There are many ways a food can make us sick: the most serious one is from immune attack after eating certain foods; but difficulty in digesting some foods or adverse reactions from toxins produced by the bugs in them can also cause sickness.
The most common confusion is between food allergy and food intolerance. But they are two completely different conditions, according to a review publication by the National Academies.
A food allergy may cause a reaction by the immune system, unlike food intolerance or food sensitivity.
An allergic reaction can be potentially severe or even fatal. They produce the IgE (immunoglobulin E) antibodies and may only require very little food to trigger an immune response. The symptoms appear within minutes to few hours, and might require immediate medical attention to serious symptoms such as anaphylaxis (which we will discuss later).
Sensitivity to food—also called food intolerance—does not involve the immune system and is rarely life-threatening. It appears when certain foods can't be digested. This happens when the body doesn't have the adequate enzymes or other means to metabolize the ingredients.
Finally, food poisoning is a result of contaminated food, e.g., from salmonella or other pathogens. It can have life-threatening effects, and should be taken seriously. 48 million cases of food poisoning occur every year, causing serious outbreaks, food recalls, and, in rare cases, hospitalizations and deaths.
The figure below shows the prevalence of respiratory, skin, and food allergies over time for children 0-17 years old. This study by National Center for Health Statistics found that both food and skin allergies increased in prevalence over time.

Figure: Trend of respiratory, skin, and food allergies over 15 years.
Some food allergies are more prone to resolve than others. For example, about 50% of children with milk, egg, or wheat allergies “grow out” of the allergy by the time they are 7 years old.
On the other hand, only about 10% of tree nut, fish, shellfish, or seed allergies in children resolve. There is no simple or accurate test that can predict the prognosis of food allergies, and regular testing might be necessary.

Figure: Likelihood of food allergies resolving as children grow up.
Anaphylaxis is a sudden allergic reaction in which symptoms occur within few seconds or minutes. Peanuts and bee stings are known to cause anaphylactic reactions that may cause skin rashes, difficult breathing, and shock to the body.

Figure: Symptoms of Anaphylaxis. Image courtesy Wikipedia commons, by Mikael Häggström.
Anaphylaxis causes the immune system to release a flood of chemicals that trigger the release of even more inflammatory chemicals. This sudden release of chemicals can cause a person to go into shock.
This shock results in drop in blood pressure and narrowing of the airways. Signs and symptoms of anaphylaxis include a weak pulse, a skin rash, nausea and vomiting, shortness of breath, and loss of consciousness.
Milk and egg are the two most common causes of anaphylaxis in children under two years old.
Preschool children have the highest rates of food anaphylaxis—and hospital admissions from food anaphylaxis. Adolescents and young adults have the highest rates of fatal food anaphylaxis.
According to a 2013 study, there were between 63 to 99 deaths per year in the United States due to anaphylaxis.
A study by Umasunthal and colleagues found that the incidence rate of food anaphylaxis in people with food allergies was 0.14 per 100 person-years. This rate varies between different age groups. For example, children ages 0 to 4 years with food allergies have an anaphylaxis incidence rate of up to 7 per 100 persons per year. That means, in a given year, up to 7 out of 100 children with a food allergy may experience life-threatening case of anaphylaxis.
There is not one comprehensive food allergy test that exists today to identify all allergies. Food allergies are diagnosed by carefully looking through medical history and by selecting tests based on this data.
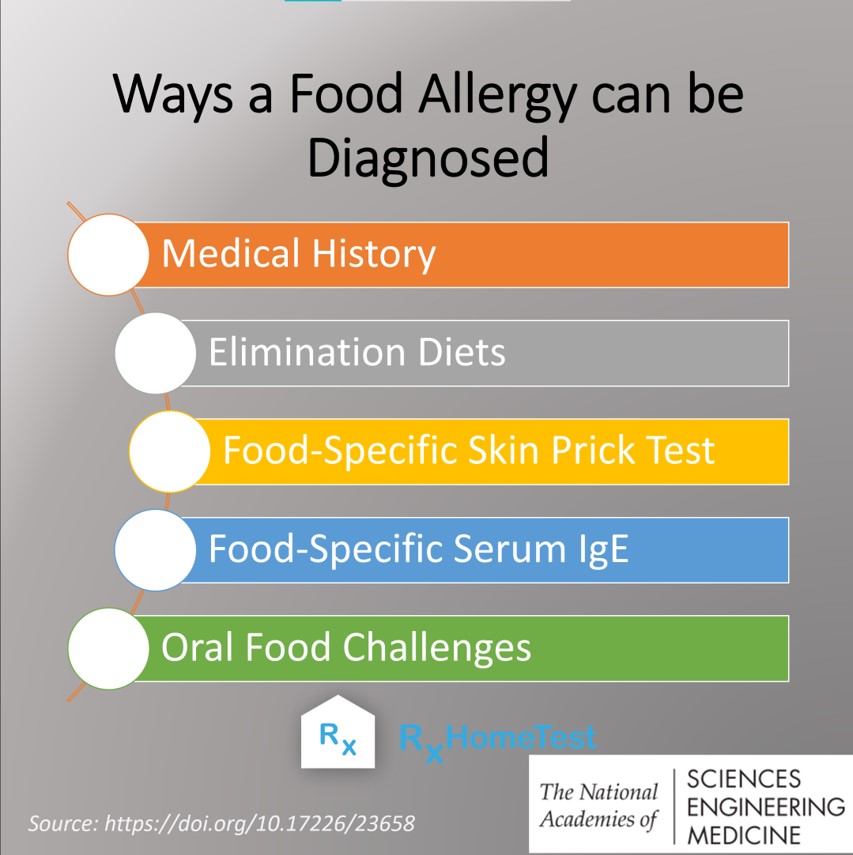
However, many testing options exist today including an IgE Test, Food Sensitivity Test, and for certain specific allergies—such as gluten intolerance— a Celiac Antibody and Genetic Test. Careful review of symptoms in children and teens can help diagnose such conditions.
One should always talk to their doctor before making a decision on what test might fit their unique circumstances.

Order a Food Allergy Test Kit.
Celiac – FAQs - key facts about gluten intolerance.
What is Celiac? History, Present and Genetic Risk - a detailed look at celiac.
Debunking the Top 5 Celiac Disease Myths - learn how to separate the facts from fiction.
Celiac Disease and Genetic Risk - a comprehensive review of the underlying genes.
Sensitivity to Food – Allergy, Intolerance, and Celiac Disease - a comprehensive review.
Food and Health: Allergies, Sensitivities, and Intolerances - learn the differences.
Food Allergies vs Food Sensitivities: What’s the Difference? - a few simple steps to differentiate.
Food Allergies and Gluten Intolerance - ways in which food can adversely affect us.
Branum AM and Lukacs SL, Food allergy among U.S. children: Trends in prevalence and hospitalizations, NCHS data brief, no 10. Hyattsville, MD: National Center for Health Statistics, 2008.
National Academies of Sciences, Engineering, and Medicine, Finding a Path to Safety in Food Allergy: Assessment of the Global Burden, Causes, Prevention, Management, and Public Policy, Washington, DC: The National Academies Press, 2017.
Jackson KD, Howie LD, and LJ Akinbani, Trends in allergic conditions among children: United States, 1997-2011, NCHS Data Brief, 2013.
Savage J, Sicherer S, Wood R, The Natural History of Food Allergy, The journal of allergy and clinical immunology: In practice, 2016.
Lee SE, Management of Anaphylaxis, Otolaryngologic clinics of North America, 2017.
Ma L, Danoff TM, Borish L, Case fatality and population mortality associated with anaphylaxis in the United States, The Journal of allergy and clinical immunology, 2014.
Umasunthar, T et. al., Incidence of food anaphylaxis in people with food allergy: a systematic review and meta-analysis, Clinical and Experimental Allergy, 2015.