Sensitivity to food varies with age but it is most prevalent in children as they start taking food after weaning. One in 20 children under the age of 5 years has some sensitivity to food. For adults, that rate is about one or two in hundred.
Most children outgrow these sensitivities as their bodies adjust to new foods. Any remaining sensitivities are often to one or two foods.
Dairy, egg, wheat and soy sensitivities are the most common to disappear over age. However, those related to peanut, tree and other nuts, fish and seafood persist over time. Only about 1 in 5 children outgrows their peanut allergies. Gluten intolerance is even harder to track as it might appear at any age and has a strong genetic pre-disposition.
Because the mechanisms behind food sensitivities are not fully understood, prevalence of food intolerance is not very clear. In a recent survey of over 40,000 US adults, 10.8% had at least one known food allergy and almost 19% believed they were allergic to some foods.

Order a Celiac Genetic Test Kit.
Celiac – FAQs - key facts about gluten intolerance.
What is Celiac? History, Present and Genetic Risk - a detailed look at celiac.
The Differences Between Genetic and Antibody Celiac Tests - and which one to order.
Food Allergies vs Food Sensitivities: What’s the Difference? - a few simple steps to differentiate.
What to Do With Your Food Sensitivity Test Results? - follow these steps to get most out of your test.
Genetic Testing and Disease Inheritability – role of genetics on health.
Testosterone and Aging – research on the male hormone.
All About Vitamin D – review of symptoms and impact.
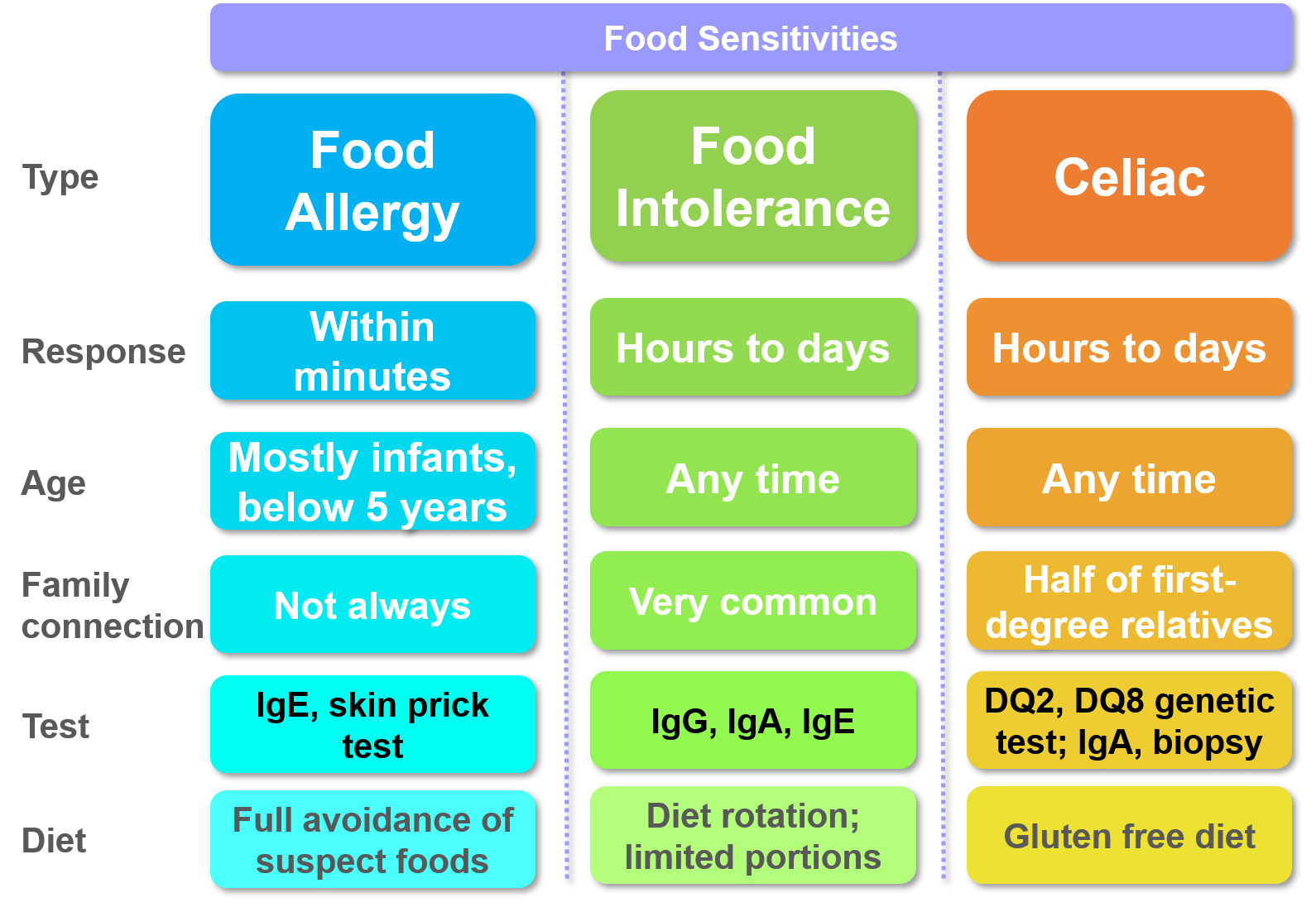
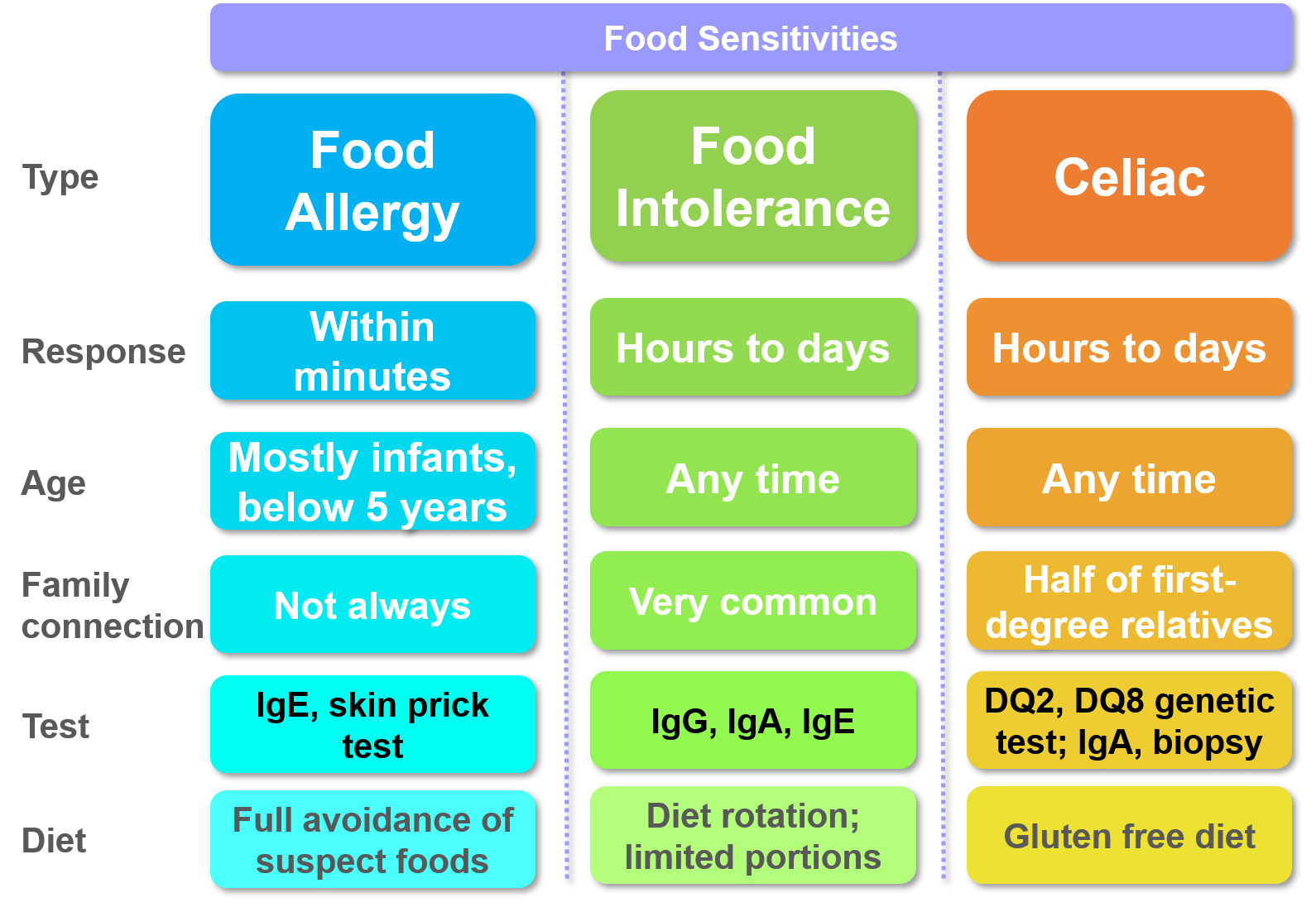
Food intolerance is slow reaction to certain foods observed after several hours or days of consuming. This delayed response and overlapping symptoms with common conditions make it difficult to pinpoint the root cause of intolerance.
In contrast, the reaction is often within minutes in case of a food allergy. In a recent survey, one in three allergic adult had visited an emergency room at least once in their lifetime. That’s why it is crucial to understand the difference between allergy and intolerance.
Food intolerance is also highly dose dependent, unlike food allergy and celiac disease where very small amounts of suspect proteins can trigger a strong reaction.
Many food chemicals, artificial coloring, preservatives, flavor enhancers, salicylates, glutamates (MSG) are known causes of food intolerance. Often a combination might make the response worse.

Response to food intolerance shows up as irritable bowl, hives, headache, migraine, fatigue, mouth ulcers, sinus congestion, irritability and mood swings. In rare cases, asthma and sudden anaphylactoid reactions requiring emergency medical care may occur. In children, irritation, red itchy rashes and reflux are common observations. These differ from food allergy, where the responses are acute and include sudden red itchy skin (hives), vomiting, difficult breathing, rapid swelling under skin (angioedema), red rashes on mouth and face (eczema) and anaphylaxis.
Celiac (Coeliac) may not show any symptoms at all. However, most common symptoms include bloating, cramps, diarrhea, constipation, fatigue, and long term impact on the body through malnutrition, anemia, and osteoporosis.
Food intolerance can occur at any age, similar to celiac disease. However, food allergies are often observed in infants when they are exposed to new foods for the first time. Adults trying completely new foods or mistakenly consuming something known to be sensitive may observe food allergies.
Family history is important in most cases and first-degree relatives of those with sensitivities are at higher risk. Family history of common symptoms of food intolerance and food allergies repeat in new cases. Chronic symptoms of asthma, eczema, hay fever, mouth ulcers, abdominal pain may repeat in family members with food sensitivities.
Celiac has a strong genetic pre-disposition to those with DQ2 or DQ8 genes. Not everyone with these genes may have celiac, but they are almost always observed in celiac patients (97% as per one study). Other auto-immune diseases, e.g., diabetes and thyroid problems also show a strong correlation to celiac.
The triggers for food allergy are specific food proteins. The culprit in celiac is gluten from wheat, rye, barley, and the wheat-rye hybrid triticale. On the other hand, food intolerance may be because of multiple reasons including food chemicals (e.g., MSG), food additives and preservatives (e.g., food coloring), certain cereals and dairy products (e.g., lactose intolerance).
In case of food intolerance, repeat consumption may not have the same reaction every time. That’s why IgG food sensitivity testing can be challenging and requires frequent and regular testing for monitoring. However, both food allergy and celiac are highly repeatable and symptoms re-appear on introduction of the suspect food.
A life long elimination of allergy triggering protein is necessary in most food allergies. Children may grow out of most allergies except few that are hard to outgrow (peanut, tree nuts, seafood). Celiac requires an adherence to gluten-free diet. In case of food intolerance, adherence to a diet below the reaction threshold of known food sensitivity might be needed.
A recent study of over 1,000 newborns suggests a mother’s microbiome affects the baby’s future allergies (Vuillermin, Nature 24 Mar 2020). Those with larger households with exposure to wide variety of diets and micro-organisms tend to have fewer allergies among kids.

The sensitivities to food vary by individuals and are often unpredictable.
A skin prick test or IgE blood test for specific protein antigen is necessary to diagnose food allergy. In case of food intolerance, an IgG test followed by elimination of suspects through a food rotation diet may help pinpoint the source of food sensitivity.
In general, eliminating suspect foods with chemicals helps. Therefore, diets low in chemicals, preservatives, flavor enhancers, artificial colors, and any naturally occurring glutamates, amines, and salicylates should be prioritized.
Once a suspect food is identified, a dietary rotation plan of repeating the food after a few days to assess the impact should be followed. A food sensitivity test can help identify the suspect foods in a diet.
Celiac may be complicated to diagnose as symptoms may never show and it may take weeks or months of gluten-free diet to become free of symptoms. However, a celiac genetic test may help assess the genetic pre-disposition–especially among families with known celiac diagnosis. If the test is positive for DQ2 or DQ8 genes, an IgA antibody test and an intestine biopsy may be necessary during diagnosis.
No one deserves to live in fear that something as common as wheat in their diet can make them sick. However, proactive checkups, adequate planning for sensitive foods, proper testing to learn about newly acquired sensitivities, and knowledge of family history of intolerances can help lead a normal life.
Food Allergy: Adverse Reactions to Foods and Food Additives, 4th edition (Chap 17: Gluten-Sensitive Enteropathy by Alberto Rubio-Tapia and Joseph A. Murray). Edited by Dean D. Metcalfe, Hugh A. Sampson, and Ronald A. Simon.
Estimated food allergy prevalence rate by Scott H Sicherer in ‘Epidemiology of food allergy’, J Allergy Clin Immunol, 2011, vol 127, page 594-602 (Food Allergy Institute of Mt Sinai School of Medicine, New York)
Prevalence and Severity of Food Allergies Among US Adults by Gupta et al in JAMA Network Open, 2019, vol 2, page e185630
Celiac Disease by Fasano et al in New England Journal of Medicine, 2012, vol 367, pages 2419-2426.
Food allergy and intolerance by Hodge, et al in Australian Family Physician, 2009, vol 38 (9), pages 705-707.
The Celiac Disease Foundation, last accessed Oct 2019.
NIH: Genetic Home Reference for Celiac Disease and Genetic Risk, last accessed Oct 2019.
Maternal carriage of Prevotella during pregnancy associates with protection against food allergy in the offspring by Vuillermin et al in Nature Communications, 2020, vol 11, page 1452.