It’s silent—and it’s a major killer.
In 2015, cardiovascular disease (CVD) was the cause of 31% of deaths (17.7 million) worldwide, according to estimate by the World Health Organization (WHO).
Recent studies show that many of those deaths are, in part, due to Vitamin D deficiency. A Vitamin D blood test and clinical measurement of blood-vessel stiffness can help assess the risk for CVD.
CVD is a combination of conditions and diseases that involve constriction or blockage of the blood vessels. Most common ones are:
Coronary heart disease – The heart’s major blood vessels are compromised.
High blood pressure – The force of blood against the artery wall is too strong.
Cardiac arrest – The heart suddenly stops.
Arrhythmia – The heart beats irregularly.
Stroke – The brain doesn’t get enough blood.
Congestive heart failure – The heart doesn’t pump enough blood.
Peripheral artery disease – Blocked arteries reduce blood flow to legs and arms.
Myocardial ischemia – A build-up of plaque obstructs blood flow to the heart.
The statistics are staggering. There were more than 400 million cases of CVD in 2015 (Roth 2017). In fact, one in every 4 deaths in the US is due to some type of heart disease, says the Centers for Disease Control and Prevention (CDC).
The main culprit for CVD is low-level inflammation of the vascular wall, known as atherosclerosis (Nitsa 2018).
It starts with deposition of lipids (LDL and unsaturated fatty acids) on the inner walls of the blood vessels. Subsequent oxidation of these lipids damages the walls. At the site of this injury, T-cells and macrophages (white blood cells) accumulate, causing more inflammation.
Over time, a build-up of plaque leads to lesions on the inner walls. This ruptures them, resulting in a host of CVD conditions, from stroke and heart attack to ischemia of the heart and other organs.
Atherosclerosis can be potentially diagnosed by a high-sensitivity C-reactive protein blood test. Early detection can help assess and, even possibly, prevent the risk of heart attack. So can a blood test for Vitamin D.
Vitamin D helps the body absorb calcium and phosphates, to build healthy bones and support muscle. It exists in several forms.
A blood test can reveal the level of the most readily available form, called 25 (OH)D or 25 hydroxyvitamin D.
On exposure to sunlight, Vitamin D converts to another form by the liver. Because Vitamin D is fat-soluble, it remains stored in liver and in fatty tissues (with a half-life of 3 weeks).
Subsequently, the kidneys convert Vitamin D to another highly active form that has a half-life of only a few hours.
Too much of it can result in Vitamin D toxicity; too little of it keeps it from doing its job.

Recent studies have shown that Vitamin D also binds to cells that have receptors for converting it into its hormonally active form, throughout the body.
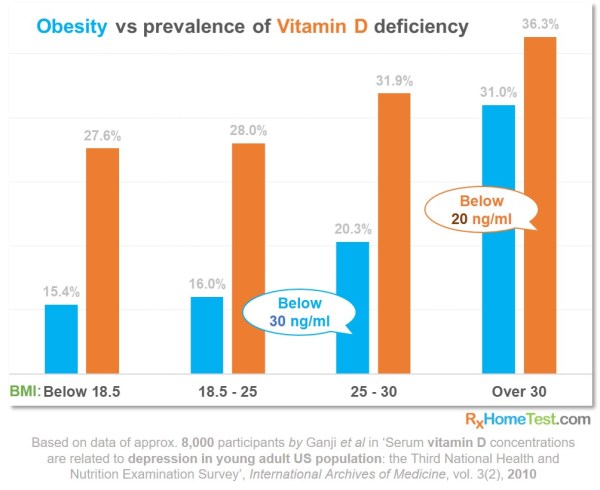
Obesity may disallow this conversion, thus lowering the levels. In 2010, an 8,000-participant study has shown that the higher the BMI (Body Mass Index) the greater the Vitamin D deficiency.
The chart below, based on this study, shows the prevalence of this deficiency. Notice how the number of participants rapidly increases with higher BMI. Here, deficient means below 20 ng/mL and insufficient means below 30 ng/mL.
A recent analysis of several research studies shows a positive correlation between Vitamin D and CVD (Judd 2009).
A higher rate of mortality observed in people living farther away from the equator (Fleck 1989). This is likely due to lower sun exposure and therefore lower Vitamin D levels .
An increase in blood pressure in people living farther away from equator (Rostand 1997Fleck 1989 – “UV light may contribute to geographic and racial blood pressure differences”).
In UK, higher death rates observed from heart disease, because of fewer hours of sunlight (Grimes 1996 – “Sunlight, cholesterol and coronary heart disease”).
A seasonally higher rates of coronary heart diseases and death in winter is noticed. That’s when there’s less sunlight, indicating its importance to human health (Douglas 1995 – “Seasonal variation in coronary heart disease in Scotland”)
Lower levels of Vitamin D (below 20 ng/mL) often associate with higher rates of heart-related issues including angina, myocardial infarction (heart attack), coronary heart disease, heart failures and peripheral vascular disease, in a US-population survey (Kendrick 2008– “Vitamin D is independently associated with cardiovascular disease in NHANES III”; Kim 2008 – “prevalence of hypovitaminosis D in cardiovascular diseases”).
Lower Vitamin D levels correlate with cardiovascular risk factors such as hypertension, diabetes, higher BMI and elevated triglycerides (Martins 2007 – “Prevalence of cardiovascular risk factors and the serum Vitamin D levels in US: NHANES III”; Scragg 2007 – “Serum Vitamin D, ethnicity, and blood pressure in NHANES III”).
Significantly low Vitamin D levels (below 15 ng/mL) show a 2-fold increase in myocardial infarction, in a 10-year follow-up of healthy men (Giovannucci 2008 – “Vitamin D and risk of myocardial infarction in men”).
Similarly low Vitamin D levels associated with a 3-to-6-times increased risk of hypertension over four years (Forman 2007 – “Plasma Vitamin D and risk of incident hypertension”).
Severe Vitamin D deficiency (below 10 ng/mL) means a 3-5-times higher risk of sudden cardiac death or heart failure, in a 7-year follow-up study of 3,000 men (Pilz 2008 – “Association of Vitamin D deficiency with heart failure”).
Vitamin D deficiency in this group results in a 50% increase in fatal stroke (Pilz 2008 – “Low Vitamin D levels predict stroke in patients”).
40% reduction in risk of Type II diabetes for those with Vitamin D levels over 28 ng/mL, from a 17-year follow-up study in Finland (Mattila 2007 – “Serum Vitamin D and subsequent risk of diabetes”).
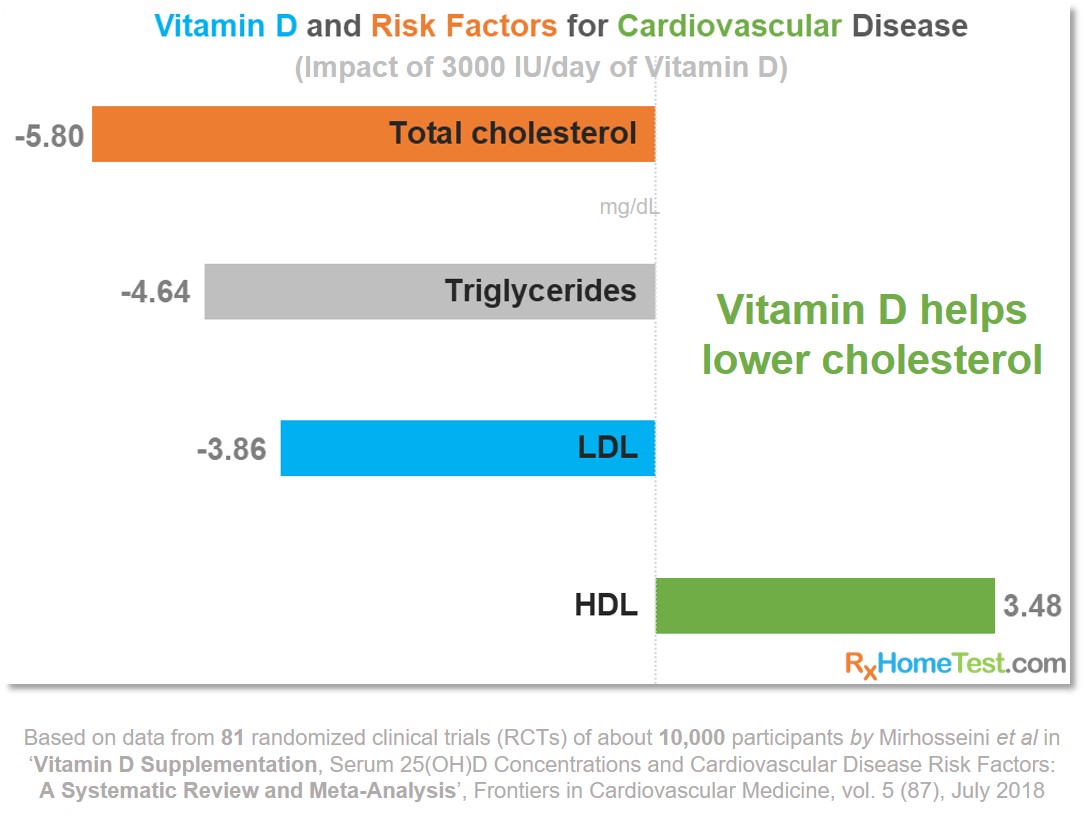
An in-depth review of 81 randomized clinical trials (RCT), comparing Vitamin D supplementation to placebos, showed that healthy Vitamin D levels help reduce the risks of CVD, as shown in the plots below (Mirhosseini 2018).
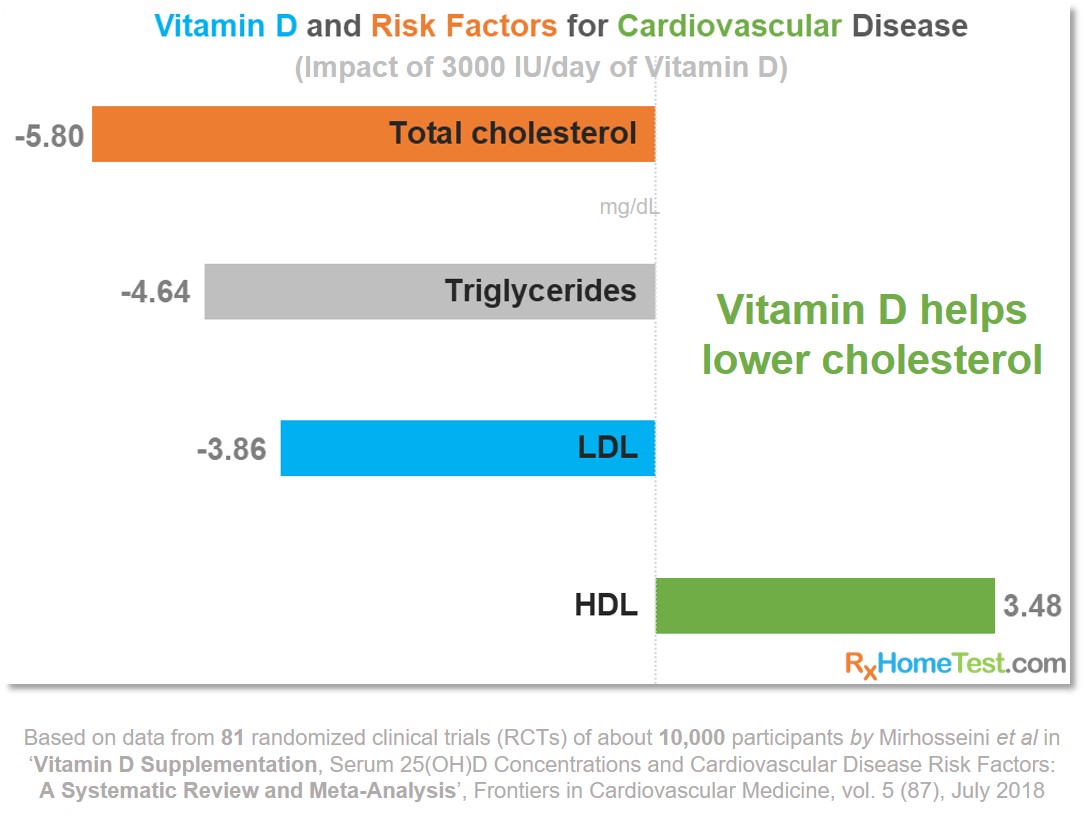
In several different studies over 25 years, with health data of nearly 10,000 participants, about half of whom were given an average dose of 3,000 IU/day of Vitamin D (individual amounts ranged between 400 to 12,000 IU/day depending on the study). Together, the studies’ results show the following:
Total cholesterol was lower on Vitamin D supplementation.
Vitamin D supplementation lowered low-density lipo-protein (LDL, or “bad cholesterol”).
Compared to placebos, significantly lower triglycerides for those taking Vitamin D .
Vitamin D supplementation saw increase in high-density lipo-protein (HDL, or “good cholesterol”).
Adequate Vitamin D levels reduced the high-sensitivity C-reactive protein, which can be tested as an independent marker for cardiovascular inflammation.
Those taking Vitamin D supplementation had lower diastolic and systolic blood pressure.
Healthy Vitamin D levels means a net reduction in parathyroid hormone, which helps maintain proper calcium balance in the blood (an excess of this hormone can cause calcium deposits in the arteries and weaker bones).

A rigorous survey by the Cochrane Review (Bjelakovic 2014 – see plain language summary on page 3) of 56 randomized clinical trials—where 95,000 participants were randomly assigned to receive Vitamin D supplementation, or no treatment or a placebo—found “some evidence that Vitamin D3 seems to decrease mortality in elderly people not dependent on help or living in institutional care.” The study concluded that “about 150 participants need to be treated over five years for one additional life to be saved;” and that “Vitamin D3 also seemed to decrease cancer mortality, showing a reduction in mortality of 4 per 1,000 persons treated for five to seven years”. However, they highlight the potential risk of kidney stone formation (seen for Vitamin D3 combined with calcium) and elevated blood levels of calcium.
An Italian study by Saponaro and colleagues—with 247 heart-failure patients compared to HOW MANY? healthy participants—showed that the patients had a 4-times-higher rate of Vitamin D deficiency (below 10 ng/mL) (Saponaro 2018).
Another study, from The Netherlands, monitored 548 heart patients for 18 months. It concludes that lower Vitamin D levels show correlation to higher rates of re-hospitalization and death, due to heart failure. Half of the study’s patients with the lower 1/3 of Vitamin D levels (below 12 ng/mL) were re-hospitalized or died. Same observation again, that only 1/3 of patients in the upper 1/3 of Vitamin D levels (above 17.5 ng/mL). The study’s data suggest about a 10% increase in rehospitalization and death for every 4 ng/mL drop in Vitamin D levels (Liu 2011).
An analysis of 7,970 participants in a US study at Georgia State University assessed impact of Vitamin D on depression. It found that almost 50% of participants had below the optimal level (30 ng/ml) of Vitamin D. Those with a “current episode of depression had 8.4% lower concentrations of serum vitamin D compared to those who did not report having depression” (Ganji 2010 – “Serum vitamin D concentrations are related to depression in young adult US population: the Third National Health and Nutrition Examination Survey”). This confirms a previous, Dutch study that “vitamin D concentrations were 14% lower in persons with major and minor depressions and that the vitamin D status was associated with both major and minor depressions” (Hoogendijk 2008 – “Depression Is Associated With Decreased 25-Hydroxyvitamin D and Increased Parathyroid Hormone Levels in Older Adults”).
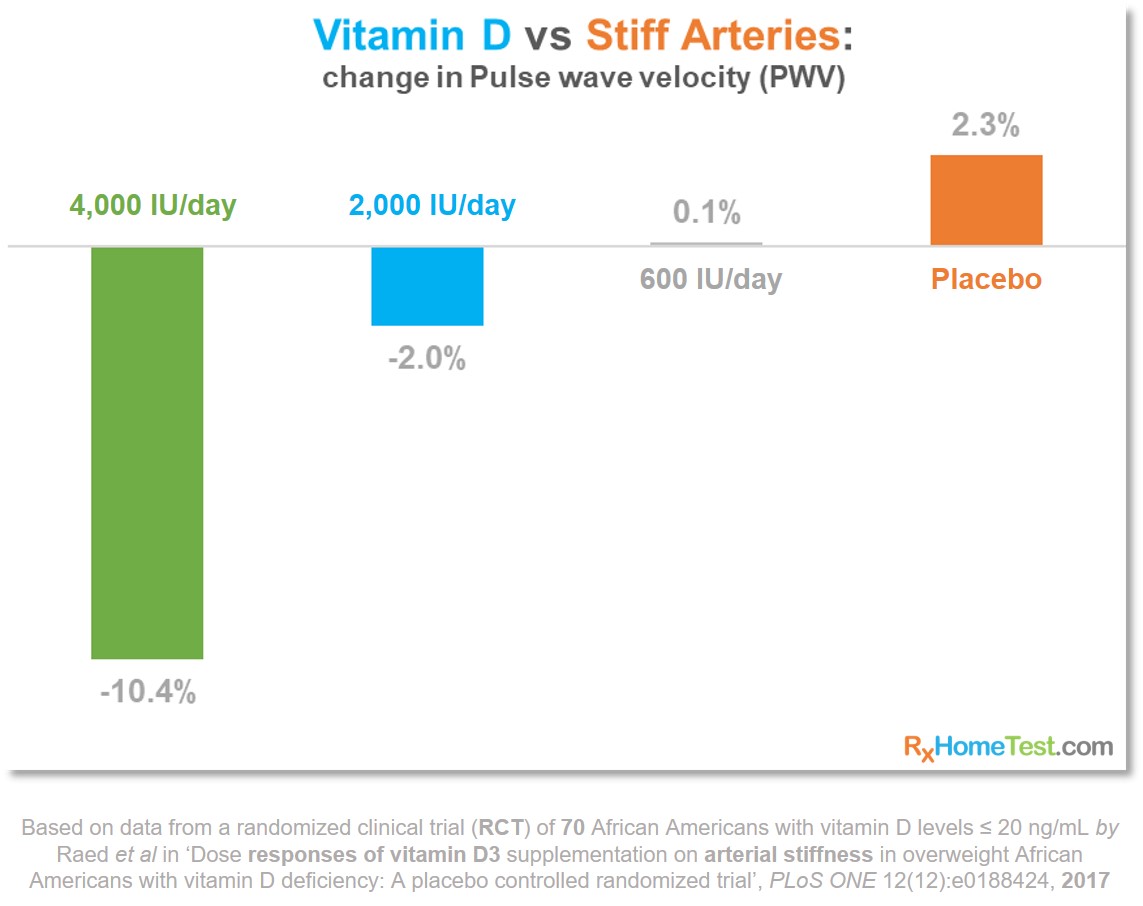
A randomized clinical trial from Indiana University studied 70 overweight African-American participants receiving varying amounts of Vitamin D supplementation over 4 months. It showed a marked improvement in arterial stiffness. To arrive at their findings, researchers used pulse wave velocity (PWV) measurements (Raed 2017 – “Dose responses of vitamin D3 supplementation on arterial stiffness in overweight African Americans with vitamin D deficiency: A placebo controlled randomized trial”).
PWV is a well-established and reliable method to quantify arterial stiffness and assess the risk of CVD. As blood flows out of the heart and into the blood vessels, it generates a pressure wave that travels along the arteries. Age, heart health and resistance built from plaque deposits inside the blood vessels affect the pressure wave. PWV uses a set of non-invasive devices to measure the rate at which this pressure waves move. The greater the stiffness in the blood vessels the higher the pressure wave velocity needed, in order to maintain adequate blood flow.
What is Cardiovascular Disease? by American Heart Association
Heart Disease by Mayo Clinic
Heart Disease Facts by CDC
Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015 by Roth et al. in J Am Coll Cardiol. Jul 2017, vol 4 (70), pages 1-25
Vitamin D in Cardiovascular Disease by Nitsa et al. in In Vivo 2018, vol 32, pages 977-981
Vitamin D Deficiency and Risk for Cardiovascular Disease by Judd et al. in Am J Med Sci. Jul 2009, vol 338 (1), pages 40–44
Vitamin D Supplementation, Serum 25(OH)D Concentrations and Cardiovascular Disease Risk Factors: A Systematic Review and Meta-Analysis by Mirhosseini et al. in Frontiers of Cardiovascular Medicine 2018, vol 5, page 87
Vitamin D supplementation for prevention of mortality in adults (Review) by Bjelakovic et al. in The Cochrane Library 2014, Issue 1 (see page 3 for plain English summary)
Serum vitamin D concentrations are related to depression in young adult US population: the Third National Health and Nutrition Examination Survey by Ganjie et al. in International Archives of Medicine 2010, vol 3 (29)
Dose responses of vitamin D3 supplementation on arterial stiffness in overweight African Americans with vitamin D deficiency: A placebo controlled randomized trial by Raed et al. in PLoS | ONE Dec 2017, vol 12 (12), page e0188424